When a patient has been registered for care in a healthcare institution, nurses form to be one of the primary groups in-charge of taking care of the said patients. In order to make sure that they are able to provide the optimum required care, nurses use a tool known as the Nursing Report Sheet.
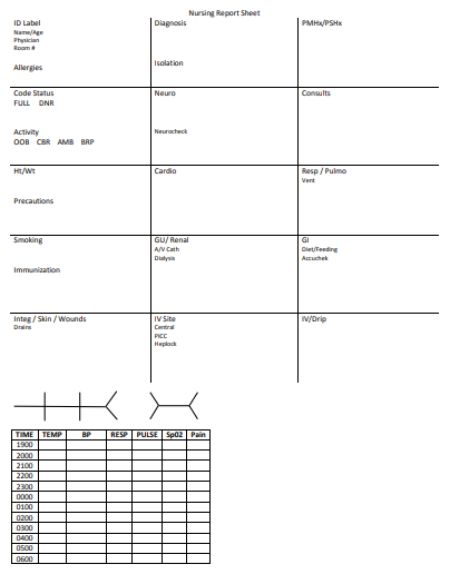
Nursing report sheets are akin to premade templates. With the help of these templates, nurses keep a track of their patient’s state at all times, whether they are in their room, ward or during ICU visits. The report sheets enable the nurses to record clear information regarding details including the diagnosis, history, allergies, consults, vital signs, lab results, and other such health-related data.
Due to their excellent recording system, nursing report sheets are used by physicians, doctors, nurses and other healthcare staff all over the world. These report sheets are highly beneficial in helping the medical staff to obtain information efficiently.
Contents
Different Types of Nursing Report Templates
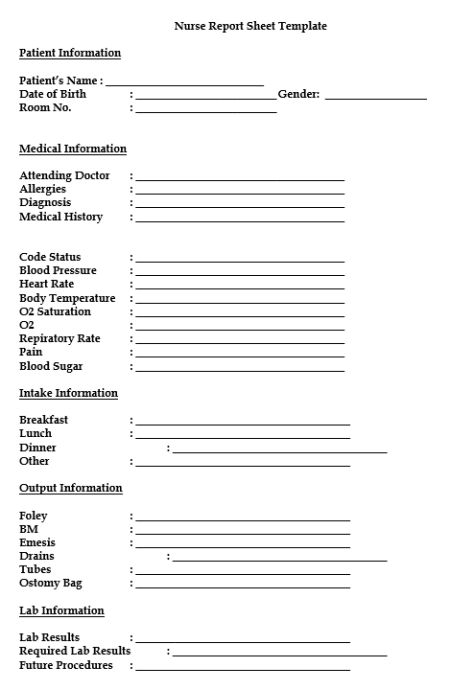
Sample Nursing Report Sheet Template
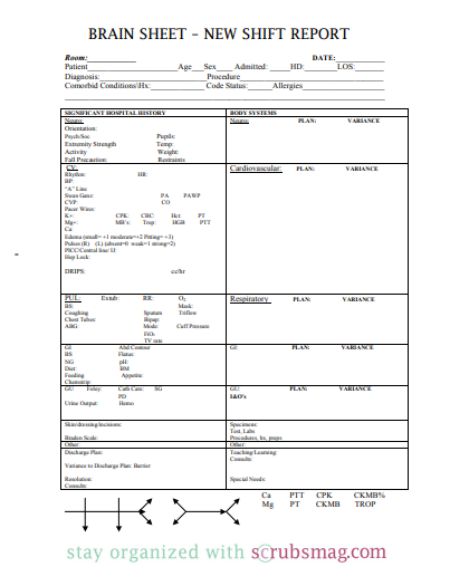
Given below is a sample Nursing Report Sheet Template which can be implemented by healthcare institutions in treating their patients.
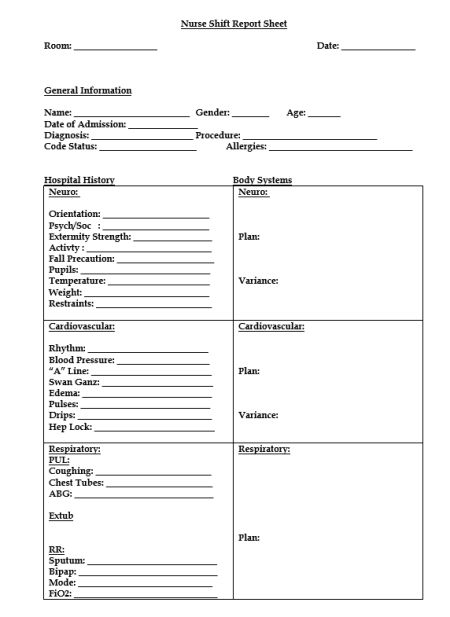
Nurse Shift Report Sheet Template
Nurse Shift Report Sheets are not not an uncommon occurrence at healthcare institutions. They are often viewed as a crucial entity that helps them to pass on patient information during routine changes in the shifts of nurses. Shift report sheets are highly useful in providing adequate information transfer, thus increasing communication levels between the nurses.
Given below is a Nurse Shift Report Sheet Template that can be implemented by healthcare organizations:
Nursing Assistant Report Sheet Template
It has always been the case that registered nurses and nursing assistants have failed to participate in optimum levels of communication. Due to this, a lot of nursing assistants fail to receive the change-in-shift or the nurse shift report sheet. In a real-world sense, this could create a lot of problems for the nursing assistants.
However, this problem can be easily solved by the means of a nursing assistant report sheet template. A nursing assistant report sheet is highly similar to the other nurse report sheet templates that have been mentioned in this article.
Given below is an example of one such nursing assistant report sheet template that can be implemented in the day-to-day functions of healthcare:
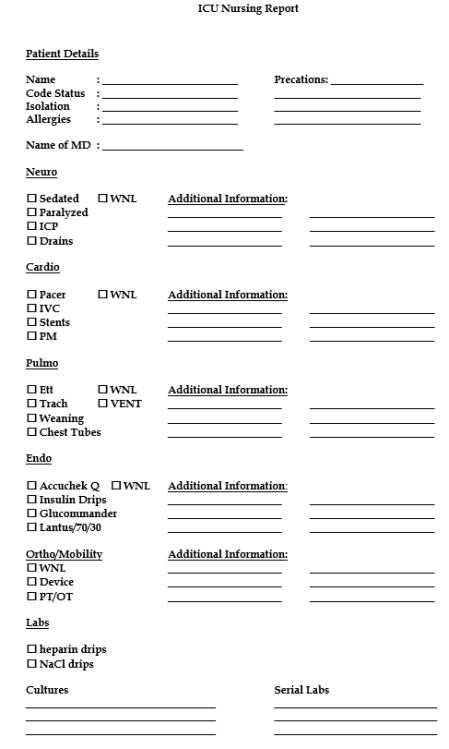
ICU Nursing Report Template
When all other treatment methods fail, ICU’s are tasked with the job of providing the required intensive healthcare to people. ICU’s or Intensive Care Units are a specialized form of treatment, tended to patients who are severely unwell. The Intensive care form of treatment is provided only to those who require the most critical of care.
At the same time, it is also highly important that nurses have an accurate knowledge of the patient’s condition. Being equipped with the knowledge of the right details allows the nurses to be empowering. Apart from this, they are also able to give accurate patient reports as and when required. Due to this, it is very important that nurses are able to gather the required information.
To help with this situation, ICU Nursing Reports were brought into action. ICU Nursing Reports are used to obtain a list of essential details regarding the patient who has been admitted to the ICU.
Given below is an example of an ICU Nursing Report:
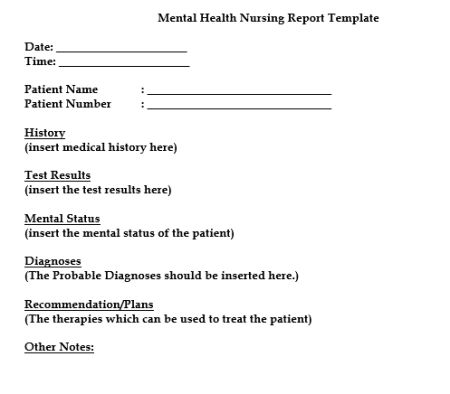
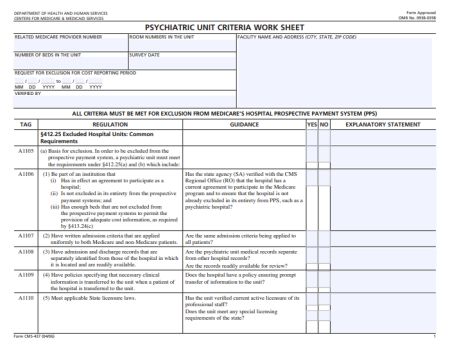
Mental Health Nursing Report Template
As defined by the World Health Organization, mental health is determined as a sustainable way of living in which everybody is able to live in a harmonious manner. In such a way of living, the people are able to cope up with the tensions that they face in daily life and still be able to produce fruitful and productive results. Such results allow them to contribute to the development of their individual community.
In the last few decades, humans have been provided by humans with a deep insight into the numerous developments made in medicine. Such drastic developments have introduced numerous innovations into the medical field, that have gone a long way in enabling healthcare providers to provide their services in an easier and safer manner. Amongst all the ingenious developments ever introduced, the introduction of the Mental Health Nursing Report was one of the pioneers that changed the way of healthcare provision forever.
Mental health nursing reports are an important aspect of the nursing handover processes. The handover process is an important aspect of all healthcare institutions. It allows nurses and doctors to continue treating and providing care to their patients even when during shift interchange. This means that, even if there is a change in the shifts of a particular group of doctors or nurses, the subsequent shift can continue providing care to their patients without any obstacles.
Being such a useful and essential part in healthcare circles, these nursing report templates are implemented by institutions all around the world. An example of the same is given below:
Components to be Included
Being highly customizable in nature, Nursing Report Sheet templates can be developed in a manner to suit the individual needs of every healthcare organization. Notwithstanding this, every report contains a few typical elements without which the report would be rendered completely useless.
Mentioned below are eight components which would, otherwise, be present in a typical Nursing Report Sheet Template. Each of these elements serves an individual purpose of their own.
The sections and their functions are mentioned in a detailed format below:
- General Information – The General Information section is the first section to be present in the Nursing Report. This section is responsible for generating all the details regarding the patient such as Date of Birth, Gender etc. of the patient.
- Patient Report – Next on the report, is the Patient Report section. The Patient Report is tasked with collecting the medical details of the patient. These details include medical details such as the Diagnosis, Allergy Information, Medical History, and Code Status.
- Patient Monitoring: Vital Signs – The Patient Monitoring section contains the vital signs that have been recorded at some particular time during their stay at the healthcare center. A few of the most important characteristics which are present in all the nursing reports are the Time Check, Blood Pressure details, Heart Rate, Temperature, Oxygen Saturation Levels, Oxygen, Respiratory Rates, Pain (if any, that has been inflicting the patient), Blood Sugar Details, Details of Dispensed Medications and Medicine Administration Timing.
- Intake – The Intake section contains information about the meals that the patient has been consuming. The sections that are recorded beneath the Intake section are Breakfast, Lunch, Supper, and Other (food that has been consumed at any other times).
- Output – Output refers to the various methods which have been employed to expel the wastes from the body. The sections which are mentioned below the Output section are Foley, BM, Emesis, Drains, Tubes and Ostomy Bag.
- Labs – Labs refers to the various patient reports which have been derived from the numerous tests conducted on the patient. The constituents of this section are Labs, Needed Labs, and Future Procedures.
- Completion – Completion is the final section of a nursing report template. This section contains the details regarding the nurse on duty. The various details to be recorded here are the Name, Signature of the Nurse and the Date and Time of the ending of the shift.ImportanceNursing Report Sheets are highly crucial in nature. This is due to their potential to house paraphernalia of significant information such as particulars of the diagnosis, medical history, allergies pertaining the patient, details regarding the presiding doctor, consults and even the duties of the nurse during their shift.However, data recording in nursing report sheets isn’t only limited to this. Their customizable nature allows healthcare institutions to add in features that enhance the features of the report sheet. This allows them to record crucial segments of information such as:
- Keeping a check of all the orders received from the doctor via telephone.
- Tracking the numerous results and other critical information that has been supplied from the lab.
- Noting down all the aspects of the food consumed by the patient as well as the wastes that have been expelled.
- Miscellaneous nursing notes to help remind nurses about the minuscule but predominant duties to be performed.
- Advance notes to prompt nurses about the duties that they need to perform in the next shift.
Moreover, nursing report sheets play a huge role in favor of the nurse’s life as well. Due to the vast expanse of the information present, a lot of nurses consider the reports to be akin to a secondary brain. Due to this, they often go into a panic-ridden state if they misplace their respective nursing sheets.
In order to make sure that they are easily accessible, a lot of nurses tend to keep the report on their person, folded within a scrub pocket or fastened on their clipboards.
Uses
The applications of a nursing report commence at par with a nurse’s shift. As soon as a nurse’s shift starts, her first priority task is to gather data from the report prepared by the previous nurse. This enables him/her to head into her assigned duties while providing clarity about task priority.
From here, the applications of a nursing report sheet get drastically varied. A few of these applications are:
- Gaining Rapid Access To Patient Information – A nursing report sheet is always present on a nurse’s body. He/she can rapidly access it whenever required. Due to this, when enquired by a doctor, he/she won’t have to fumble while recollecting the details of the patient. He/she can simply pull out the nursing report and read out the details of the patient from the nursing report sheet.
- Keeping A Track of Tasks – As they go through their day-to-day activities, we often find that nurses have to perform a lot of duties during their shift. A nursing report sheet enables these nurses to keep a track of the tasks that they have to perform. This allows them to go through their activities, in an untroubled manner and without missing out on any of the tasks.
- Differentiating The Patients – Traditionally, healthcare institutions are assigned to take care of vast numbers of people. It is, therefore, not surprising that doctors and nurses often get confused amongst the sheer number of patients. A lot of people might argue that nurses have to, at most, take care of 6-7 people. In spite of this, it is natural for nurses to get confused amongst these patients.
A nursing report sheet prevents this from happening. They enable the nurses to differentiate amongst their assigned patients with the help of several details such as the patient diagnosis, histories and so forth.
- A Basis for An Accurate Charting – Charting is one of the most important aspects of any healthcare institution. It allows the providers to keep a record of several important aspects such as medical history, demographics, vital signs, diagnoses, medications, treatment plans, progress notes, immunization dates, allergies etc.
A nursing report makes all of this possible and more. With the help of a report, healthcare institutions can create an accurate charting system. Such systems can systems which are easier to read as well as create. Even during the situations of patient load, there charting systems are not laid to a halt and still tend to function properly.
Q&A
Q1. How do you write a good nursing report?
A1. A nursing report is created to facilitate the job of transferring information. Therefore, it is highly essential that the nursing report is created in a manner that successfully fulfills its objective. Given below are a few tips which all nurses keep in mind to create a near-perfect nursing report:
- A Consistent Format – Consistency is the most factor when it comes to writing a nursing report. As much as possible, employ a consistent format system. A consistent format system makes the nursing times, several times easier to read. Simultaneously, it also assists other nurses to rapidly distill the required necessary information simply by skimming through the report.
- Punctuality – Make it a habit to pen down all the notes gathered within 24 hours of supervising the patient. Formulating down the notes allows you to put attention to the numerous details and aspects, of the patient’s condition, while they are still fresh laden in your memory. Formulating down the notes within 24 hours serves a multi-fold purpose. As the details are fresh in your memory, you can curb the possibility of any errors from being transferred.
- Encapsulate redundant information – Those nursing reports are considered to the most beneficial which house only the necessary details regarding the patient’s condition. Everything apart from this is to be considered redundant and should be mandatorily excluded from the report. Apart from this, you should also check and remove other details which have absolutely no connection to your patient’s health.
- Simplicity – Simplicity is an important aspect of life. Such is the case with a nursing report as well. Nursing reports are created, keeping in mind, the quick extraction of crucial information. They are created in a manner so that doctors and nurses are able to gather data simply by skimming through the report. To make this possible, make sure that you write the report as simple as possible. You shouldn’t venture deep into the patient’s medical history. Only include the information that is extremely important vis-a-vis the patient’s health.
- Implement Standard Abbreviations – Refrain from using abbreviations. As far as possible, try to write the content in complete terms. This prevents the nursing report from becoming too complicated. If you really need to use them, implement standard abbreviations that are determined according to medical guidelines. The usage of medical terminology in abbreviations allows nurses and doctors to be familiar with the terms and easily read through the report.
- Write Legibly – Traditional methods involve nursing reports to be written by hand. There are institutions who do employ computed methods for creating a nursing report. However, if your institution emphasizes the use of handwritten nursing reports, make sure that your handwriting is legible. Clarity and legibility in your handwriting provide a quick and effortless transfer of information amongst the doctors, physicians, and nurses. Apart from this, legibility drastically in the number of errors caused due to the provision of incorrect medication. A lot of cases witness patients undergoing fatal consequences due to wrong medication generated from illegible reports.
Q2. What is ‘reporting’ in nursing?
A2. In medical circles, reporting refers to the act of transferring relevant information. In most cases, this information refers to the patient information that is transferred from one nurse to another during the change of shift. There are numerous occasions that require reporting. The most common of such are the occasions in which a patient is being transferred or when the shift of a nurse or doctor ends.
Traditionally, a nursing report is used as a means to perform nursing. Nursing reports are peer-reviewed journals used to facilitate the easy access of research data amongst other nurses and physicians. These reports ensure that patient information is easily available whenever required.
Q3. What is an end-of-shift report?
A3. End-of-shift reports are created by compiling previously recorded patient information. As suggested by their name, these reports are written by nurses as they wrap their shifts ups. End-of-shift reports are responsible for lodging numerous important details. A few of these are:
- The patient’s medical situation
- A brief history
- The medication needs
- Details of allergies
- Pain levels etc.Such important aspects enable end-of-shift reports to enhance communication levels between co-workers and team members. Aside from this, the reports also ensure proper execution of tasks, situation control and complete oversight on the entire condition of the patient.
Q4. What is handover in nursing? A4. The definition of the term handover is akin to the term end-of-shift. Handover refers to the process of communication that occurs between the nurses of two non-identical shifts. In this process, the nurses communicate information about patients that are kept under the care of the nurses.
Q5. Do nurses have to write reports?
A5. Yes. All the reports that are communicated during the handover process are written explicitly by the nurses.
Q6. What is a flow sheet in nursing?
A6. In simple terms, a flow sheet is a single or dual-page form, tasked with the job of gathering all important aspects of a patient’s condition. Similar to the other nursing reports, the flow sheet is tasked with gathering patient information. This flow sheet is housed within the patient’s chart and is used to gather a reminder of the care to be provided and the record to denote whether the set tasks have been performed or not.
However, the main goal of a flow sheet is completely different from other nursing reports. A flow sheet is brought into play every time a medical practice hits a dead end. Whenever the doctor hits a dead end in their treatment procedure they can easily refer to the flow sheet to address the patient’s ailment.
Q7. What is a progress report in nursing?
A7. When a patient is registered for care at a healthcare institution, he or she has to deliver some information that can be used for treating his health. Apart from this, the treatment procedure requires numerous negative as well as positive outcomes to be noted in relation to the patient. To make sure that all this information is stored safely to be used in the future, doctors use progress reports. Progress reports are essentially journals that can record all types of situations.
Q8. What should be included in a nursing incident report?
A8. Also known as an occurrence report or event report, an incident report is a formal piece of document that has to be filled in the event that a person meets up with an unfortunate incident at a healthcare institution.
There are two main reasons for writing a nursing incident report:
- To inform the healthcare facility about the incidents that have occurred.
- To alert the insurance company for the need for further investigations.
To make sure that there is sufficient information for both the healthcare facility as well as the insurance company, an incident report should contain the following details:
- The circumstances leading to the event.
- The exact details of the incident. A few such details include the date, time and location at which the incident occurred.
- Any witnesses who might be able to provide further clarity in the incident.
- The methods applied to provide remedy the incident.
- Vital signs of the patient.
- Injuries sustained.
- Environmental hazards which contributed to the incident.
- The presence of faulty equipment which led to the cause of the incident.
- The origin of any new risk factors that might have arisen due to the incident.
- The remedial actions that were undertaken towards reducing the possibility of another incident.
Q9. Why is documentation so important in nursing?
A9. The ultimate goal of writing nursing reports is to encourage documentation activities. The sheer volumes of reports generated are enough to suggest that documentation is a highly important aspect of nursing. There are various characteristics which contribute to the importance of documentation. These include:
- Access to clear and accurate documentation.
- Promotion of a nursing environment that safe, quality and evidence-based.
- Efficient communication levels that ensure continuity of care.
- Create databases which can map the effective rate of treatment.
- Planning and evaluation to aid the treatment of the patient.
Q10. Why is nursing writing important?
A10. Writing is a crucial segment of nursing. It is highly expected for nurses to correctly portray their words and properly communicate all the information. There are various reasons which make nursing writing highly important. These include the ability to communicate in a professional manner, sharing of thoughts, sharing of knowledge etc. Apart from this, writing in nursing is used on a daily basis to communicate about the known observations.
Details of allergies