During a client-doctor relationship, healthcare professionals often come across large amounts of helpful information. This information is often quite helpful in the foreseeable future. However, it is not possible to retain all such information in memory. Therefore, in order to cope with this shortcoming healthcare professionals make it a habit to take down notes citing their interaction with their clients.
we are providing an awesome collection of SOPA Note Counselling Templates that are useful for any type of health professionals and health providers. Feel free to have a look at our document which also gives you complete information about SOAP Note Counselling Template. All our templates are free to download and easy to use. Free printable and customizable templates available absolutely free.
Contents
Developing a SOAP Note
Given below are a few sample statements which can be used while developing a SOAP note.
- Subjective – The Subjective section contains a summary statement that is given by the client. Traditionally, this statement is preferred to be recorded in the form of a direct quote. Few samples of this could include:
- “My lower jaw has been hurting for a couple of days.”
- “I start to break down when he yells at me. What should I do?”
- “I have been avoiding sugary snacks. But it has been difficult as I just quit smoking.”
- Objective – The Objective sections contains data which matches with the statement, previously made by the client. Most commonly, this section houses the various changes or problems which the client has been going through. A few samples of this are:
- Late to the session. Slouched body posture. Uninteresting in the group session.
- Vitals: Blood Pressure – 122/78. Body Temperature – 98.7. HR – 72 Regular
- Clinical Exam Results: Extraoral – No symmetry or swelling. Intraoral – Eruption of the supra, occlusion on the pericoronal tissues, fetid odour, pain to palpation etc.
- Assessment – The Assessment section contains a judgment of the situation that the patient is going through. Various other factors could also be included in this section such as details about the session, situation etc. Even the most obvious of the assessments are not excluded. A few samples for which could be included in this section are:
- Needs support for dealing with (the situation)– Needs to take responsibility for being on time to the group meetings.
- Asthmatic – exercise-induced asthma
- Diabetes – A1C is not at target

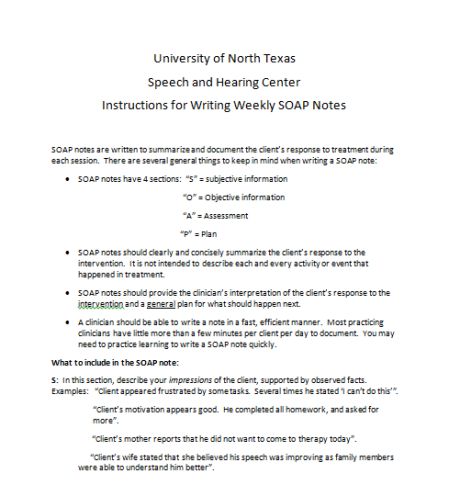
Plan – The final section i.e. the Plan section contains the planning to be implemented for any future clinical requirements. This section should mandatorily review the intervention to ultimately lead to the development of the treatment plan. A few samples which could be included in this section are:
- Consider a mental health evaluation referral.
- Administering antibiotics for 10 days and evaluating the results.
- Encouraged to book an eye check-up.

SOAP Samples
SOAP Note Template for Counseling
Given below, are few SOAP note templates which can be used in counselling.
Template No. 1:
Patient Name – ______________________________________
Practitioner’s Name – _________________________________
Date: ___________________
SOAP Notes
- S – Subjective:
ID: (Brief details regarding the patient)
Chief Complaint (CC): (Use patient’s primary report in the form of direct quotes in quotation marks)
History of Present Illness (HPI): (Include details such as onset, duration, progression, timing etc. of any past occurrences of the present illness)
Current Medications: (Include all the medications that the patient is taking)
Social History/Habits: (Social habits such as smoking, consumption of tobacco, drugs, alcohol etc. should be recorded)
- O – Objective:
Vital Signs: (Vital Signs that haven’t been listed elsewhere)
General Observations: (Does the patient appear to be in anxiety, pain or any other observation can be noted down here)
Physical Examinations: (Include only those examinations which are relating to the chief complaint)
Diagnostic: (List of results that you already have)
- A – Assessment:
Diagnosis: (The Diagnosis should be written according to the level of your understanding of the problem and the subjective and objective data)
- P – Plan:
Diagnostic – (In this part, you have to write about the X-rays, lab and other tests that you plan for the patient)
Treatment –
Education –
Consultation –
Follow-up –
Doctor’s Signature – _______________________________
Date – _____________________
Template No. 2:
SOAP Note
Patient’s Name: ______________________________ Date: __________________
- Subjective
Client Compliants : __________________________________________________________
Symptoms: _________________________________________________________________
Medication Which Improve Symptoms: __________________________________________
Medications which Worsen Symptoms: __________________________________________
- Objective
Visual Observations: _________________________________________________________
Test Results: ________________________________________________________________
Modalities Applied: __________________________________________________________
- Assessment
Changes Achieved: ___________________________________________________________
Diagostics: __________________________________________________________________
Goals Set: __________________________________________________________________
- Plan
Treatment Plan: _____________________________________________________________
Self-Care Plan: ______________________________________________________________
Doctor’s Signature: _____________________________
Date: __________________
Example for SOAP Notes for Counseling

Patient Name – ______________________________________
Practitioner’s Name – _________________________________
Date: ___________________
SOAP Notes
- S – Subjective:
ID: 56-yr old woman. Widowed. Works as a waitress. Generally healthy.
Chief Complaint (CC): “Burning feeling in the stomach.”
History of Present Illness (HPI): “Burning feeling started two months ago. Night-time discomfort. An occurrence of nausea and bloating.”
Current Medications: None, presently.
Social History/Habits: Denies smoking, drinking or drug use. Exercises at least 3 times each week.
- O – Objective:
Vital Signs: N/A.
General Observations: N/A.
Physical Examinations: Abdomen is soft and protuberant. There are no masses or tenderness. No striae or bowel sounds. No rubs.
Diagnostic: N/A.
- A – Assessment:
Diagnosis: Usage of antacids and H2 blockers.
- P – Plan:
Diagnostic – Avoid food that makes symptoms worse.
Treatment – N/A
Education – N/A.
Consultation – Seek medical advice if symptoms seem to worsen.
Follow-up – Return again if treatment needs to be further assessed by the doctor.
Doctor’s Signature – _______________________________
Date – _____________________
Progress Notes in Counseling


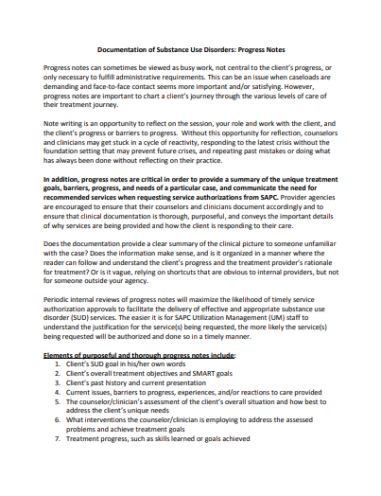
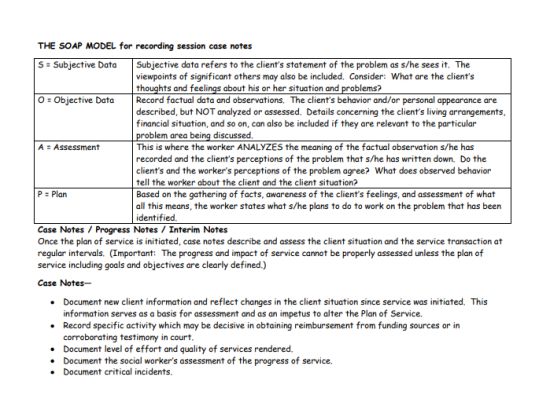
In counselling, progress notes are used to measure the progress of a particular treatment being administered. There are various components which go ahead in creating a progress note including the assessment, diagnosis and the treatment protocols involved in the procedure. Besides this, progress notes also keep a record of the methodologies that have been implemented by the practitioner to take care of any undue crisis that might have arisen in the midst of the procedure.
Developing a progress note requires numerous forms of data. A few of such include:
- The required medication that has been prescribed and the results that have been derived from such prescription.
- The frequency at which the treatment has been furnished to the patient.
- The results obtained from the clinical tests.
- Summary of the diagnosis, functional status, symptoms and the progress to the current.
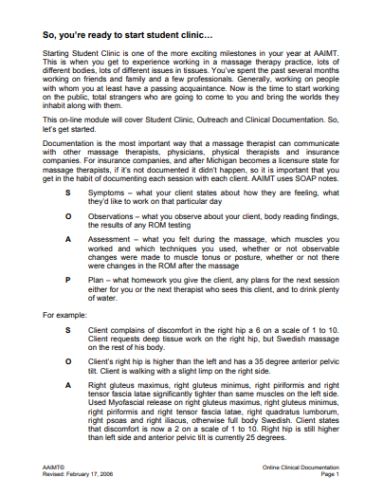
The perfect examples of progress notes are SOAP. A SOAP note consists of four sections, namely: Subjective, Objective, Assessment and Plan. Each of these sections is employed for assessing the problems of the patient and furnishing him with a form of treatment. Apart from this, the DART form of note-taking notes is also an efficient way of recording the progress of a patient. DART stands for Description, Assessment, Response, and Treatment.
Progress notes are highly used by physicians as well as nurses. With the help of progress notes, healthcare providers are able to easily document the care provided to their patients.
What Are SOAP Notes in Counseling
SOAP originated from another method of note-taking known as the POMR. POMR or the problem-oriented medical record was developed by Dr Lawrence Reed, a pioneer in the field of note-taking. In the decades passed since its origins, SOAP has been used by uncountable healthcare professionals.
The primary reason for the SOAP method’s popularity is its proven results in real life. The note-taking method has been tried and tested to be highly successful by counselling professionals. In spite of the origins of other methods, SOAP is still the fundamental method of note-taking being used all around the world.
The Importance of Note-Taking

The primary function of note-taking is undoubted, memory-retention. Apart from this, the activity also serves various other advantages. On a daily basis, professionals vastly implement note-taking in counselling in their day-to-day routine. Such professionals range from psychiatrists, psychiatric nurses, psychologists, counsellors etc.
Note-taking increases in significance when patients seek treatment from multiple healthcare providers. The multiple healthcare providers usually reference the key points that have been voted down by the previous provider. A lot of times, these key points allow the professionals to provide further care to the clients without the hassle of going through the processes again.
It is due to such advantages that provokes healthcare professionals to actively involve themselves with note-taking procedures. However, the process in itself can become a very messy task.
And this is what led to the origins of the SOAP methodology. SOAP stands for Subjective, Objective, Assessment and Plan. It is a format of note-taking which is used all over the world by professionals to document client information in a structured and organized manner.
The Components of a SOAP Note
The content being housed in SOAP Notes are vary depending on the clinical situation. However, in all the cases, there are some similarities such as the patient’s name, healthcare provider’s name as well as the attending physician’s name. Apart from this, the note also contains four major sections.
Akin to its acronym, a SOAP note comprises of four sections. These are, namely, S – Subjective, O – Objective, A – Assessment and P – Plan. An elaborate description of these four sections are given below:
- Subjective – The Subjective section is the first section of a SOAP note. Often referred to as the chief complaint, this section contains the reason for the client’s visit to the professional in the form of a brief statement. Usually, this statement is noted down in the form of a direct quote by the client.
- Objective – The Objective section generally contains quantifiable details regarding your client made according to your observations from your point of view. The details could comprise of numerous factors such as:
- Results determined by physical exams
- Measurements of vital signs
- Changes in behavioural health such as foul odour, rapidity in speech, quickness in eye movements etc.
- Involvements of other systems such as cardiac and respiratory systems etc.
Although most of the factors are easy to interpret, behavioural health is one area in which all the work is interpretive. The details recorded beneath behavioural health is not as objective as other details such as the results determined by vital signs or measurements of vital signs.
- Assessment – The Assessment section performs the function of housing the diagnosis. In a gist, the Assessment section contains all the conclusions drawn up in regards to the time spent between the patient and the provider. A lot of times, the section also contains information that is referenced from previous interactions.
If required, the healthcare provider can also opt to include a differential diagnosis within the section. There are conditions which bring forward numerous symptoms posing similarly to other diseases. Due to this, the healthcare provider lacks the definitive quality required for assessing them correctly at the first go.
- Plan – The final section of the SOAP note comprises of the Plan section. This section is used to contrive a programme the healthcare provider or practitioner will go through to help a patient through their concerns. This plan is used to develop an evidence-based plan for further treatment.
However, it should be kept in mind that this section of a SOAP note is not a treatment plan alternative. The Plan section sets goals or tasks for therapy or disease-state monitoring parameters. Due to this, this section is often written in a shorthand format. The aforementioned tasks could serve numerous purposes such as referrals to other professionals, undertaking follow-up sessions with the practitioner etc.


How To Write Progress Notes for Mental Health

Apart from counselling, another area of the medical industry which hugely relies on SOAP notes is in the treatment of mental health. In order to write a progress note for mental health, there are several factors which the practitioner needs to keep in mind. These include:
- Conciseness – The first aspect which the provider needs to keep in mind is conciseness. He/she should document all the necessary information but avoid any irrelevant details.
- The inclusion of Adequate Details – Conciseness does not mean that you should exclude the important details as well. Make it a point to include critical information that is required for explaining treatment decisions.
- Take Care While Treating Suicidal Patients – While treating a patient with suicidal tendencies, take care to contain well-reasons explanations for any course of treatment that you pursue. If a patient commits suicide after your treatment, your progress note may be your only defence against a malpractice claim.
- Write Legibly So That Other Clinicians are Able to View the Note as Well – Write legibly so that other people can read them without frustration or annoyance. Apart from this, also remember that other clinicians will tend to read your notes. Make sure that they are able to read the note properly and administer the proper treatment.